You have put (approximately) 40 weeks of pregnancy behind you, gone through the long hours of labor and delivery and are finally a mother. Congratulations! Now begins the transition from pregnancy to postpartum, which brings with it many new questions and symptoms.
In many European countries, postpartum or pelvic floor physical therapy is the STANDARD OF CARE to help new moms navigate the weeks following childbirth. Unfortunately in the United States it is often harder to initiate these important services. Progress PT wants to make sure our patients past and present know that we are here for them and their needs.
Post-partum physical therapy can help with:
- Urinary retention, urgency, frequency & incontinence
- Constipation & fecal incontinence
- Painful intercourse
- Diastasis Rectus Abdominus
- Restoring core strength and return to exercise
- Pelvic, low back, and hip pain
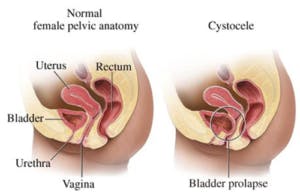
- Pelvic organ prolapse prevention or treatment
Symptoms such as those listed above can occur both during and after pregnancy. If any of the above resonate with you, don’t delay in coming for an evaluation. Ideally, postpartum care for all mom’s would begin with a screen 6-8 weeks after delivery, but our therapists can help new moms at any stage of their recovery!
Good exercises after delivery:
- Gently engaging your pelvic floor muscles as if you were going to hold back gas or stop the flow of pee
- Diaphragmatic or “belly” breathing
- Light aerobic exercise like walking or elliptical for 20-30 minutes
- Yoga For Pelvic Floor video from Yoga with Adrienne on YouTube

Remember, the postpartum period is a time to be kind to yourself and body. If any of the above are causing pain, discomfort or coning of the abdomen, schedule with your pelvic floor PTs at Progress before continuing.
Contact your US Representative today to advocate for postpartum care!
There is currently a bipartisan bill being introduced in the US House of Representatives fighting for postpartum care for Medicaid patients. The Optimizing Postpartum Outcomes Act (H.R 8181) designates pelvic floor physical therapy services as a treatment option covered under Medicaid and the Children’s Health Insurance Program (CHIP). If the bill is passed, funding would be allocated towards establishing best practices for providers to follow and screening and referral tools to get patients where they need to be faster. Even better, this bill and the funding included would require the Department of Health and Human Services to educate providers AND postpartum women about the need for pelvic health and pelvic floor physical therapy after baby. How amazing is that! The hope is that if a federal insurance program starts providing postpartum care, private insurance companies will start picking up on the importance of offering the same services to their clients.
How to advocate:
- Find out who your US Representative is. This website is super helpful! https://www.house.gov/representatives/find-your-representative#:~:text=If%20you%20know%20who%20your,the%20U.S.%20House%20switchboard%20operator.
- Go to the website of said US Representative and find their Contact tab.
- If email is available, copy and paste the below information into the body of the email.
- Submit! Yay, you’ve just advocated for pelvic health services!
Email body:
Please consider cosponsoring the Optimizing Postpartum Outcomes (OPO) Act (H.R. 8181), legislation which raises awareness of the availability and importance of pelvic health services, particularly pelvic health physical therapy, for postpartum women using Medicaid and CHIP. This legislation was introduced by Reps. Jaime Herrera Beutler (R-WA) and Lisa Blunt Rochester (D-DE).
Pelvic health physical therapy is a vital part of recovery in the postpartum period. It can aid in muscle control, tissue repair, and help heal internal portions of cesarean section and perineal scars. However, many mothers lack access to and awareness of the benefits of pelvic health physical therapy. Even some health care providers may not be aware of the importance of pelvic health physical therapy in the postpartum period.
As federally and tax funded agencies, it is important that Medicaid and CHIP recipients and providers are aware of the services to which they have access. Failure to receive timely pelvic health physical therapy could result in postpartum mothers developing life-long conditions that may have physical, mental, and financial consequences. This legislation would ensure Medicare and CHIP recipients and providers are aware of and using this vital care.
H.R. 8181 is designed to address knowledge and access gaps by providing guidance to state Medicaid and CHIP programs administering pelvic health services performed during the postpartum or neonatal period. It also authorizes programs to raise both provider and patient awareness of the importance of pelvic health examinations and pelvic health physical therapy.
Pelvic health physical therapists diagnose and treat individuals across the gender spectrum and lifespan for pelvic health related conditions that include, but are not limited to urinary dysfunction, bowel dysfunction, musculoskeletal dysfunction, sexual dysfunction, cancer-related rehabilitation, and the peri-partum state. After performing an evaluation and making a diagnosis, Pelvic Health Physical Therapists create and implement personalized plans based on best available evidence to help their patients improve mobility, recover from injury, prevent future injury, and manage pain and chronic conditions. They are part of a collaborative care team aimed at empowering patients to be active participants in their care and well-being. We must ensure that patients in need of pelvic health understand its importance and know they have access to it when needed.
I urge you to promote the well-being of postpartum mothers by co-sponsoring H.R. 8181. Thank you for your consideration.