Physical Therapy and Radical Prostatectomy
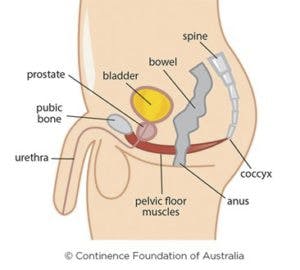
An estimated one-sixth of men will suffer from prostate cancer in their lifetime. Radical prostatectomy is the most common therapy for prostate cancer, but often leads to urinary incontinence (UI). In fact, it is reported that up to 80% of men have UI one month post-operatively, and 30-45% continue to have UI at one year. Pelvic floor muscle training is a common conservative treatment to address UI in men and women. Multiple studies have reported on the effectiveness of this approach; most recently, a 2019 meta-analysis published in the Asian Journal of Andrology. Wu, et al. found that the best available and most current research demonstrates pelvic floor muscle exercise guided by a physical therapist post-operatively decreases urinary incontinence and increases quality of life for patients at early and long-term stages. A study by Goode, et al published in JAMA in 2011 shows the efficacy of patient education + individualized physical therapy exercise to reduce the number of incontinence episodes in men with persistent urinary incontinence 1-7 years post-radical prostatectomy.
At Progress PT – Midlothian, our clinicians have specialized training in both oncological rehabilitation and care of the male patient. We apply tools such as pelvic floor muscle re-education, strengthening, and coordination utilizing biofeedback, rehabilitative ultrasound imaging and manual therapies to assist patients in regaining control. Because recovery from prostate surgery/cancer also has an impact on patients’ psychosocial livelihood, comprehensive education as well as use of restorative yoga and diaphragmatic breathing improve our outcomes. Topics may include proper voiding behavior, stress management, common bladder irritants, body mechanics for lifting, as well as nutrition to improve bowel elimination. Our goal is to treat each patient as an individual so their treatment will be unique, as we help them return to activities such as marathon running, golf, gardening and more without worry.

